When pregnancy sickness becomes something more
What is the pregnancy sickness spectrum and how do I know if I have hyperemesis gravidarum (HG)?
What is the pregnancy sickness spectrum?
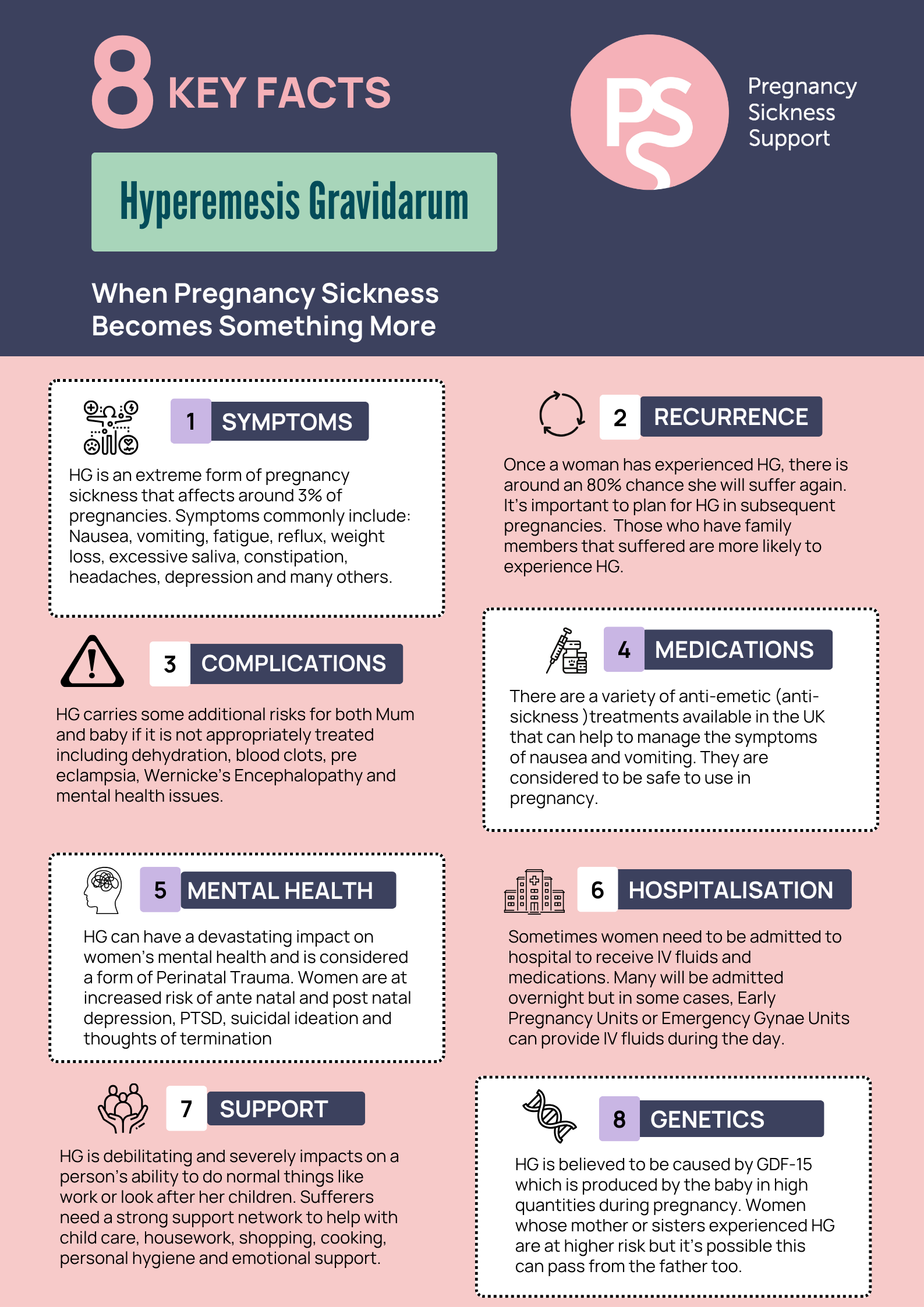
While up to 90% of pregnant women and people experience some level of nausea and vomiting in pregnancy (NVP), HG is a severe form of pregnancy sickness that sits at the extreme end of the pregnancy sickness spectrum. It affects around 3% of pregnancies each year and can lead to dehydration, weight loss, and serious physical and emotional distress.
Mild to Moderate NVP
What is Mild – Moderate NVP?
Also referred to as morning sickness (though this is an outdated term, as symptoms can occur at any time of day), mild – moderate nausea and vomiting in pregnancy (NVP) usually allows you to continue with your normal daily activities without too much disruption, but it can still be unpleasant. Symptoms typically ease by the second trimester.
You may lose a small amount of weight, but you’re generally able to stay hydrated, as you can keep fluids down. Your symptoms may be episodic—you might struggle to eat or drink at certain times in the day, but are able to make up for it when you feel better later.
Common self-management strategies such as eating little and often, resting when possible, and avoiding strong smells or certain foods can help ease your symptoms.
However, if you’re unable to keep anything down for long periods, are losing weight, or feel that your symptoms are severely impacting your daily life, this may be a sign of something more serious like Hyperemesis Gravidarum (HG).
If you’re unsure, always seek help.
What is HG?
The Windsor definition (2021) characterizes HG as “a condition that starts early in pregnancy, before a gestational age of 16 weeks, and is characterized by severe nausea and/or vomiting, inability to eat and/or drink normally and strongly limits daily activities.”
Other HG facts and indicators.
- Up to 30,000 pregnancies per year in the UK are affected by HG.
- Diet and lifestyle changes will not help alleviate symptoms.
- May begin very early, even before a positive test.
- Symptoms peak at 9-13 weeks, can improve around 16-24 weeks.
- Weight loss may be severe and rapid, and dehydration is common.
- If not managed appropriately complications can ensue.
- Medical treatment is necessary.
- Psychological support is beneficial.
- Spectrum condition, not all HG looks the same.
- 1 in 5 people with severe HG will have symptoms throughout their whole pregnancy.
If you want to know more about HG and the potential genetics surrounding the condition you can read more below.
What do I do if my daily life is being impacted by NVP or HG?
It’s not always easy to pinpoint exactly where you are on the spectrum of pregnancy sickness, but as soon as you are struggling then it’s time to seek support.
Early intervention with treatment can help to prevent your symptoms from deteriorating and you don’t need to wait until things become desperate before you seek help.
Don’t delay in seeking help because you feel like a burden, or too “weak” to be dealing with “morning sickness”.
Many women and pregnant people will never have a formal diagnosis of HG, but regardless of this, if you are struggling then you deserve help.
Dehydration
It is important that you seek medical treatment if you are unable to keep any food or fluid down as you can become dehydrated very quickly. IV fluids/medication may be required in order to stabilise your symptoms.
Some symptoms of dehydration to be aware of:
Dry lips
Dry mouth
Thirst
Reduced urine output
Darker urine
Headaches
Low blood pressure
Dizziness
Please contact your GP, Midwife or local Early Pregnancy Unit for advice.
In an emergency call 111 for immediate advice on where to travel to in your area to get treatment.
What now?
Step 1 – Speak to a Healthcare professional
If you are struggling with NVP, or if you believe that you have HG, it’s important that you speak to your GP or Midwife as soon as possible.
Untreated pregnancy sickness or HG can lead to complications for both you and your baby.
Nausea on it’s own can be debilitating and is enough to warrant treatment if it’s having an impact on your ability to eat, drink and generally function as normal.
Malnutrition, dehydration and other complications from nausea and/or vomiting must be treated by a healthcare professional.
Step 2 – Find out about treatment options
It can feel scary or unnerving to think about taking medications during pregnancy.
Please be assured that there are decades of information and research on medications and treatments currently available for NVP and HG.
You can read about those here. Or you can contact us to talk through any concerns you might have.
Your doctor should always consult with you on the risk vs benefit of untreated NVP and HG and as a patient you have a right to be equally involved in any decisions made about your care.
Step 3 – Contact us for support and information
With over 20 years experience of supporting those suffering with NVP and HG and their families, we have a wealth of information and guidance.
We are striving to ensure that pregnancy sickness is better recognised and understood amongst healthcare professionals, but there is still work to be done and it is sadly common for those suffering to find themselves dismissed.
If this happens to you please get in touch with our support team and we can help.
Please note that the information on this page is for guidance only and is not medical advice.
“The baby growing in the womb is producing a hormone at levels the mother is not used to. The more sensitive she is to this hormone, the sicker she will become.“
Professor Stephen O’Rahilly | University of Cambridge