Planning for an HG pregnancy
If you’ve suffered hyperemesis gravidarum before then unfortunately the chances are you will suffer again. But we can help.
Planning for another pregnancy…
If you’ve suffered hyperemesis gravidarum before then, unlike with regular pregnancy sickness which can differ in each pregnancy, the chances are you will suffer again; in fact, research suggests if you have had HG before then there is an 89% chance you will get it again. Therefore, planning and preparation is key to reducing the impact of the condition, particularly if you now have small children at home.
If your previous pregnancy ended with loss, either through termination or miscarriage it is important you take time to grieve and come to terms with the loss before heading back into a tough nine months. Please visit our HG & Loss page for more support.
Also, if there is trauma or anxiety remaining from the previous pregnancy then take time to recover and seek help with this before moving onto another one. Consider therapy or counselling with us.
Helpful Resources
We have produced some documents to help you prepare for a hyperemesis pregnancy, which are available to download below.
Preparing for an HG pregnancy
This is a preparation document which helps you to reflect on your previous pregnancy, look at what worked, what didn’t and what could be done differently this time. You can use this to have a discussion with your doctor prior to, or at the start of, a subsequent pregnancy.
HG Care Plan
This care plan is designed to be completed with your GP or consultant; it is in a “doctor friendly” format that they will hopefully recognise and respond to. You can ask that this plan goes into your patient held maternity notes and a copy can be scanned for your GP/hospital notes so that any doctor or midwife can access it.
Pre-emptive Treatments
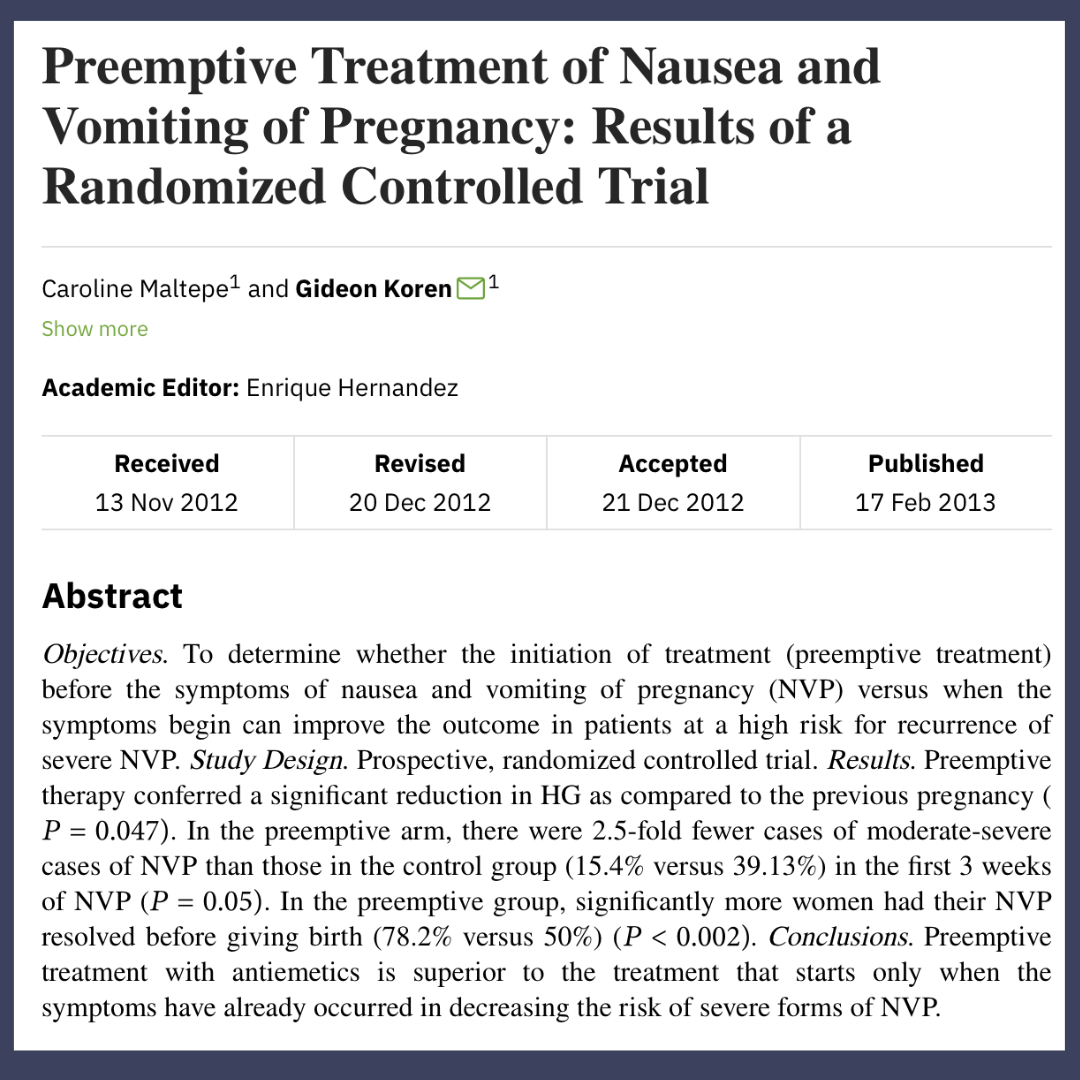
There is good evidence that the early, pre-emptive use of a vitamin B6 supplement and a first line medication is effective for preventing the deterioration which results in hospital admission. Speak to your GP about using this treatment if you have suffered hyperemesis gravidarum in the past. A 2013 study found a significant decrease in severity of HG if treatment was started BEFORE symptoms start compared to started when symptoms first appear.
Ideally you need to have an appointment with a GP who understands your previous pregnancy and who can support and put together a management plan with you. Once the plan is in place you can ask the GP to put this into your maternity notes so that all doctors and midwives must follow it. You can ask your GP and consultant to communicate to ensure your care and treatment is more cohesive.
If you are struggling to receive pre-emptive treatment please contact us.
Planning Tips
- Childcare is really helpful. Whether it is through friends and family or formal childcare with a nursery, child-minder or nanny, it is important that you’re able to rest and concentrate on staying hydrated and nourished as much as possible.
- Prepare meals for the freezer. Whilst planning your pregnancy get as many meals in the freezer as possible to avoid having to cook so much during your pregnancy.
- Stock up on drinks/foods you like and were able to tolerate last time.
- Get support! Contact our support team in advance so that we are ready to help you when the time comes.
- Eat well and take supplements including folic acid in the lead up to pregnancy, so that if you do become unwell and find it difficult to keep food/supplements down then you will have a good base level in your system.
- Contact your GP, midwife and any other professionals that will be involved. Explain that you want a plan in advance, discuss what worked and didn’t work last time, give permission for partner/relatives to discuss care if needed.
Pregnancy Sickness Support: Q1 Impact Blog 2025
Reflecting on a powerful start to the year As we step into the second quarter of 2025, we're proud to reflect on the incredible impact our small but mighty team has had in just the first three months of the year. Support Services: Reaching More...
“I was so scared to try for another baby. The PSS team were the listening ear I needed.”
Jeanette Wilshire | Blackburn
