After paralyzing nausea and intractable vomiting caused her to lose the baby she was carrying in 1999, Marlena Fejzo decided to use her professional skills to understand her personal tragedy. A geneticist at the University of California, Los Angeles, Fejzo began to research hyperemesis gravidarum (HG), an extreme form of the “morning sickness” that afflicts most pregnant women. Jeopardizing the health of mother and fetus with dehydration and malnourishment, the little-studied condition hospitalizes at least 60,000 U.S. women a year.
Now, two studies, one led by Fejzo, suggest that an excess of a blood-borne protein, growth differentiation factor 15 (GDF15), is a cause of HG, and perhaps other cases of nausea and vomiting in pregnancy. The finding “finally gives some answers … and validates what women have been experiencing,” says Caitlin Dean, a U.K. nurse who became chair of a patient advocacy group after enduring unrelenting vomiting and nausea when pregnant multiple times. In the past, some doctors asserted that women exaggerated their symptoms, and even today, women with hyperemesis report that medical staff brush off the severity of their symptoms as a routine part of pregnancy.
Dean, who now studies HG as part of a Ph.D. program at the University of Plymouth in the United Kingdom, calls the GDF15 discovery “an incredibly exciting breakthrough” that proves HG is a physical, not a psychological, condition. The finding “also points to potential therapeutic intervention,” says biochemist Stephen O’Rahilly of the University of Cambridge in the United Kingdom, who led the second study, which independently highlighted GDF15.
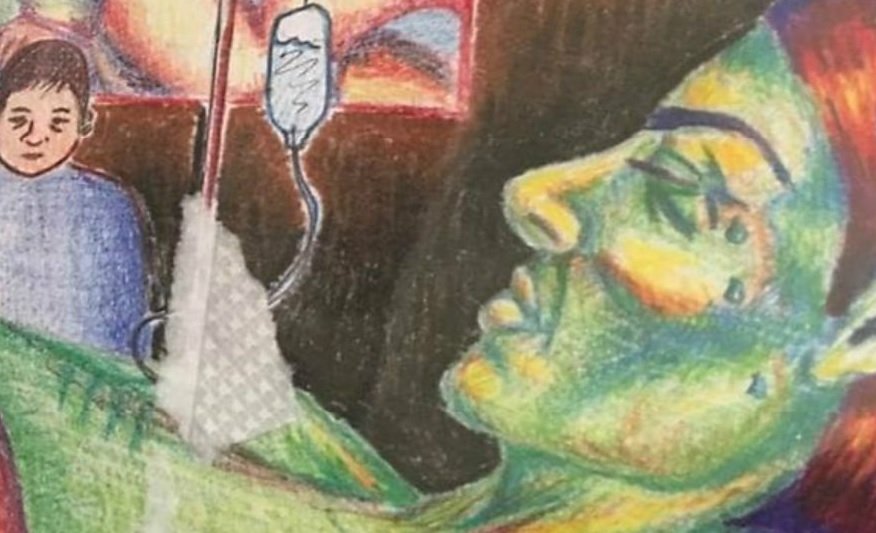
Unable to keep food and liquids down as early as 4 weeks into a pregnancy, women with HG can lose more than 5% of their normal body weight. They suffer electrolyte imbalances, vitamin deficiencies, and other symptoms of starvation that can lead to blood clotting dysfunction and brain atrophy. Violent vomiting can produce complications such as esophageal rupture and retinal detachment. Symptoms peak around 9 weeks’ gestation, but can persist until birth. The traumatic experience can lead women to end a pregnancy or decide not to have more children.
Some studies have implicated estrogen and pregnancy hormones in HG. Fejzo, whose initial research focused on cancer genetics, has slowly built a case that genes play a role in the condition. In 2007, she persuaded the consumer genetic testing company 23andMe to incorporate questions about pregnancy sickness into its surveys, enabling her and her colleagues to scan the genomes of thousands of the company’s customers for DNA variations associated with hyperemesis.
That partnership paid off. In Nature Communications this week, Fejzo’s team reports two genome-wide association scans. One compares the genomes of 1306 women who received intravenous (IV) fluid therapy for nausea and vomiting during pregnancy—a proxy for HG—to those of 15,756 who did not report any nausea or vomiting while expecting. Two variants stood out, the most significant associated with the gene for GDF15 and the second with a gene for a protein called IGFBP7. Previous animal studies suggest that both molecules influence placenta development and appetite.
In the second analysis, the team scrutinized the genomes of pregnant women reporting a gradient of nausea and vomiting symptoms, from none to very severe. The same DNA variants stood out. Finally, Fejzo confirmed the results in a non-23andMe cohort of hundreds of women with hyperemesis who required IV fluid therapy or a feeding tube. The genome scans didn’t implicate estrogen or other hormones. Fejzo’s study shows “very clearly that genetic variation close to GDF15 is the single, strongest genetic signal for hyperemesis,” O’Rahilly says.
Last year, O’Rahilly’s team reported in a preprint that women who said they had vomiting during the second trimester had more GDF15 in their blood at 12 to 18 weeks of gestation than those who reported no nausea and vomiting or only feeling nauseated. That finding, he suggests, connects GDF15 to more typical pregnancy sickness, and perhaps to HG as well.
The molecular link makes sense to Samuel Breit, an immunologist and physician at St. Vincent’s Hospital in Sydney, Australia. His team has previously found cancer patients with an anorexic and muscle-wasting syndrome called cachexia also have high blood levels of GDF15. Such patients experience persistent nausea and extreme vomiting as well. Last year, another group found that knocking out GDF15’s receptor in the brain made mice resistant to chemotherapy-induced nausea.
These clues have sparked interest in blocking the actions of GDF15 for therapy, O’Rahilly says. Fejzo and other researchers caution that it’s too soon to consider testing such a strategy in expectant women, given how little is known about the protein’s role in pregnancy. Reduced serum levels of GDF15 are associated with miscarriage, so the molecule may confer some protective effect—perhaps by keeping the mother from consuming potentially toxic foods. But Dean is optimistic. “At least there is hope now for the future,” she says.
https://www.nature.com/articles/s41467-018-03258-0